dr Laurent Goubau
WAT IS HET?
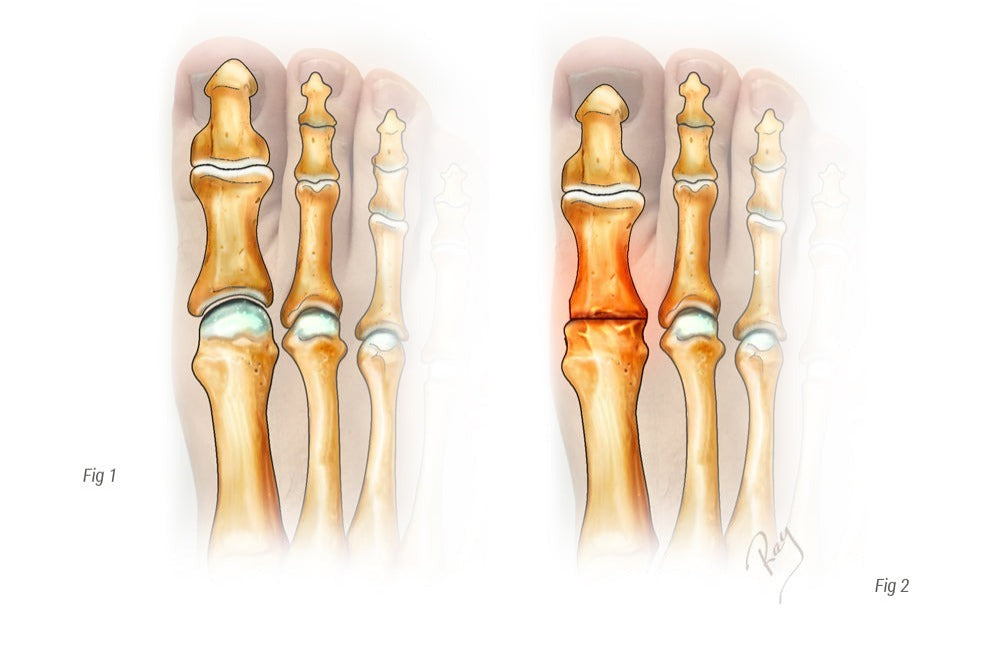
Hallux rigidus is artritis van de grote teen (ook wel hallux genoemd), meer bepaald het gewricht tussen het middenvoetsbeentje en de falanx. Artritis wordt gedefinieerd als slijtage van het kraakbeen, het gladde witte weefsel dat het bot bedekt. Kraakbeenverlies is helaas onomkeerbaar. Het zorgt geleidelijk voor verstijving van het gewricht en veroorzaakt snelle veranderingen in de mobiliteit (het wordt stijf). De progressie van de ziekte wordt gekenmerkt door de ontwikkeling van gezwellen of botuitsteeksels rond het gewricht, die we osteofyten noemen. Dit resulteert in een mechanisch conflict tussen deze uitsteeksels of, wanneer ze groot zijn, een direct conflict met de schoen en de uitsteeksels. Drie soorten ongemak kunnen optreden bij deze aandoening: verlies van mobiliteit, gewrichtspijn en de ontwikkeling van osteofyten.
KLINISCHE PRESENTATIE
Meestal is de beweeglijkheid van de grote teen aanzienlijk verminderd en kan deze pijnlijk zijn bij mobilisatie of dorsaalflexie, wanneer het kootje in conflict komt met de osteofyt.
Als de osteofyt groot is, ontstaat er directe wrijving met de schoen, wat zeer invaliderend is.
WANNEER MOET U EEN SPECIALIST RAADPLEGEN?
Verminderde mobiliteit is meestal geen reden voor een consult. Bij aanzienlijke pijn bij bewegingen of bij het aantrekken van schoenen is het raadzaam een specialist te raadplegen.
Het klinisch onderzoek wordt afgerond met een radiologisch onderzoek om de positie van de osteofyten te lokaliseren en de ernst van de aandoening te bepalen.
NIET-CHIRURGISCHE BEHANDELING
Omdat de pijn voornamelijk wordt veroorzaakt door de beweging van de grote teen, bestaat de behandeling uit het zoveel mogelijk beperken van de beweging. Dit kan worden bereikt met behulp van een stevige steunzool of door schoenen te dragen met een inlegzool die de voet soepel laat bewegen. Comfortabele schoenen worden aanbevolen om de pijnlijke directe druk op de osteofyt te beperken.
Het gebruik van ontstekingsremmende medicijnen kan tijdelijk pijnverlichting bieden. De meeste van deze behandelingen hebben echter een beperkt effect.
CHIRURGISCHE BEHANDELING
Wanneer conservatieve behandeling niet voldoende is, moet een operatie worden voorgesteld.
Er zijn verschillende opties mogelijk, afhankelijk van de mate van kraakbeenbeschadiging en de ontwikkeling van de osteofyten.
Wanneer de slijtage van het kraakbeen gering of matig is en het grootste probleem de osteofyten en de conflicten die daarmee gepaard gaan betreft, kan een eenvoudige excisie uitstekende resultaten opleveren.
Deze techniek, cheilectomie genaamd, wordt meestal uitgevoerd door een open excisie van de botuitsteeksels. Soms wordt dit type operatie aangevuld met een ingreep aan het bot ter hoogte van de falanx, om de dorsaalflexiemobiliteit verder te verbeteren (osteotomie van de falanx).
Het is belangrijk om op te merken dat deze techniek het kraakbeenoppervlak niet aantast. Artrose, en daarmee de slijtage van het gewricht, ontwikkelt zich onafhankelijk. Deze chirurgische ingreep lost het probleem van het osteofytenconflict op en herstelt een zekere mate van beweeglijkheid van de grote teen. Het biedt tijdelijke verlichting van de pijn, maar is soms voldoende om de definitieve blokkade van het gewricht (= artrodese) jarenlang uit te stellen. In feite zijn alle gewrichten omgeven door een hard omhulsel, een kapsel genaamd, dat onder spanning staat van de osteofyten en de druk op het gewricht verhoogt. Na een cheilectomie neemt deze druk af en neemt de belasting van het gewricht af.
Wanneer de kraakbeenbeschadiging te ernstig is, is de voorkeursoperatie het definitief blokkeren van het gewricht. Deze procedure, artrodese genaamd, bestaat uit het verwijderen van het resterende kraakbeen, het tegen elkaar plaatsen van de twee botten en het fixeren ervan met een plaat of twee schroeven. In tegenstelling tot wat vaak wordt gedacht, heeft het blokkeren van het gewricht weinig gevolgen voor de kwaliteit van leven en kunnen de meeste patiënten na genezing weer sporten (75-95%, afhankelijk van de sport). Het dragen van hoge hakken kan een probleem zijn, maar patiënten waren vóór de operatie meestal gestopt met het dragen van dergelijke schoenen vanwege het verlies aan mobiliteit door de artritis.
Postoperatieve follow-up
Bij een operatie waarbij de osteofyten (cheilectomie) eenvoudigweg worden verwijderd, is lopen direct toegestaan op comfortabele schoenen. Fysieke activiteiten kunnen worden hervat zodra de pijn het toelaat. Het ziekteverlof duurt 2 tot 6 weken, afhankelijk van de postoperatieve ongemakken en het type werk dat u doet.
Na een artrodese is belast lopen direct toegestaan, gedurende zes weken beschermd door een speciale schoen. Een wandelstok mag uitsluitend voor comfortdoeleinden worden gebruikt.
Autorijden kan na zes weken weer hervat worden. Wanneer er slechts één voet geopereerd is, mag er na kortere tijd weer autorijden, mits het een automaat betreft.
Afhankelijk van het beroep (zittend of actief werk, staand werk of niet, etc.) is het 3 weken tot 3 maanden duren voordat u weer aan het werk kunt.
Wat betreft de sport kunt u na 8 weken beginnen met zwemmen of fietsen; hardlopen of contactsporten vereisen minimaal 3 maanden.
RISICO'S EN COMPLICATIES
Naast de mogelijke complicaties na elke vorm van chirurgie (trombose, infectie <1%, algodystrofie <1%), wordt erkend dat de behandeling van hallux rigidus de volgende risico's en complicaties met zich meebrengt:
- Terugkeer van gewrichtspijn of osteofyten bij een eenvoudige cheilectomie. Artritis verandert niet door deze operatie en de natuurlijke progressie ervan bepaalt de progressie van de pijn.
- Niet-consolidatie van de artrodese (pseudartrose). Deze mogelijke complicatie vereist een revisieoperatie.
- Zenuwbeschadiging (meestal tijdelijk en regressief)
- Aanhoudende zwelling (oedeem). Normaal gedurende de eerste 2-3 maanden, maar kan in sommige gevallen langer aanhouden.
