dr Laurent Goubau
WAT IS HET?
Metatarsalgie betekent letterlijk pijn (=algie) onder het/de middenvoetsbeentje(s) onder de voorvoet. Het kent vele oorzaken en een specifiek klinisch onderzoek bepaalt meestal de oorzaak, waarna een gerichte behandeling kan worden voorgesteld.
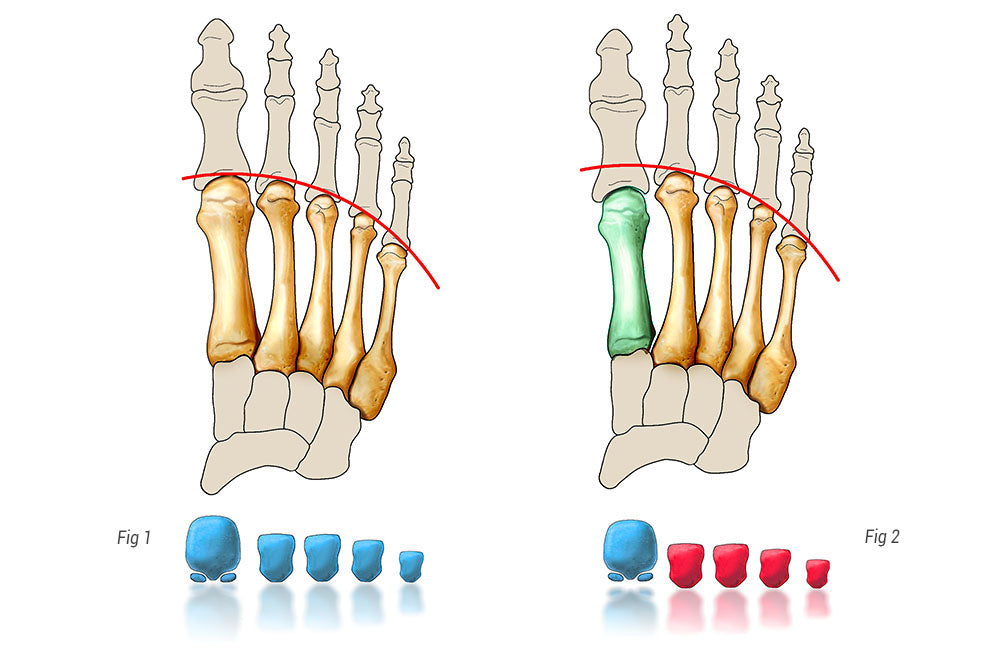
Het lichaamsgewicht wordt verdeeld over de vijf middenvoetsbeentjes (botten in de middenvoet, verbonden met de tenen). Het eerste bot, verbonden met de grote teen, krijgt 2,5 keer meer gewicht dan de andere. De rest van het gewicht wordt vervolgens verdeeld over de andere middenvoetsbeentjes. Elke onbalans in deze verhouding veroorzaakt een cascadeverandering, wat betekent dat er een extra belasting op een of meer van de andere middenvoetsbeentjes valt. Pijn ontstaat dan specifiek onder de overbelaste middenvoetsbeentjes.
Onder de zogenaamde metatarsalgie kunnen zich nog andere pathologieën verbergen: een stressfractuur van het middenvoetsbeentje of -kootje, een ruptuur van de stabiliserende plantaire structuur van de metatarsofalangeale gewrichten, een ontwrichting van de teen, de vorming van hamertenen,…
Er kunnen meerdere oorzaken aan dit probleem ten grondslag liggen. De overdruk kan te wijten zijn aan een verkorte achillespees, een anatomisch te lang of te steil (van opzij gezien) middenvoetsbeentje ten opzichte van het andere, een leeftijdsgebonden doorzakking van de voorvoet, vaak in combinatie met hallux valgus, bij bepaalde hoge wreefvoeten, bij bepaalde neurologische aandoeningen,…
KLINISCHE PRESENTATIE
De pijn bevindt zich altijd onder de kopjes van de middenvoetsbeentjes en uitsteeksels zijn gemakkelijk te voelen aan de basis van de tenen, met of zonder eeltvorming (harde huid). Eeltvorming is vaak een relevant klinisch teken en kan zeer lokaal aanwezig zijn, bijvoorbeeld onder het kopje van het tweede middenvoetsbeentje, of meer verspreid over de gehele voorvoet. Zolang de overdruk onder het middenvoetsbeentje niet wordt aangepakt, zal het eelt zich opnieuw ontwikkelen.
Metatarsalgie is een stressgerelateerde pijn die wordt veroorzaakt door overdruk op een specifieke plek.
Traditioneel is het tweede middenvoetsbeentje het eerst aangedaan. De pijn neemt meestal toe overdag bij het lopen en langdurig staan; de pijn vermindert bij rust en neemt toe bij het dragen van hoge hakken.
WANNEER MOET U EEN SPECIALIST RAADPLEGEN?
Als de pijn aanhoudt ondanks het beperken van de overbelasting, of als de pijn invaliderend wordt, is het raadzaam een specialist te raadplegen. Een uitgebreid en specifiek klinisch onderzoek helpt bij het stellen van een juiste diagnose en het aanbieden van de juiste behandeling.
Het onderzoek wordt doorgaans afgerond met een radiologisch onderzoek, om de diagnose te verfijnen en de oorzaak van de aandoening te bepalen.
NIET-CHIRURGISCHE BEHANDELING
De behandeling is in principe niet-chirurgisch. De druk op de voorvoet kan worden verminderd door de kuitspieren te ontspannen met behulp van rek- en strekoefeningen van de gastrocnemiusspier (achillespees). Op maat gemaakte orthopedische of podotherapeutische inlegzolen kunnen eveneens de druk onder de verschillende middenvoetsbeentjes herverdelen. Soms, in zeer specifieke gevallen, kan een infiltratie, gevolgd door 6 weken tapen, enige verlichting bieden.
CHIRURGISCHE BEHANDELING
Indien deze behandelingen niet voldoende zijn, kan een operatie worden overwogen. In ieder geval moet de gehele voetfunctie in ogenschouw worden genomen. Deze behandeling kan afzonderlijk worden uitgevoerd of in combinatie met andere chirurgische ingrepen:
- Verlenging van de gastrocnemius-spier aan het proximale deel van het been;
- Overdracht van een buigpees;
- Hechting van de stabiliserende plantaire plaat;
- Bij een hallux valgus of varusafwijking van de grote teen dient deze aandoening eveneens operatief te worden gecorrigeerd.
- De meest voorkomende ingreep is een osteotomie (open of percutaan), waarbij de druk op het/de middenvoetsbeentje(s), verantwoordelijk voor de overdruk, wordt verlicht door het een paar millimeter in te korten, of door het iets op te tillen, of door een combinatie van beide. Na een dergelijke osteotomie wordt meestal een schroef geplaatst om ervoor te zorgen dat de vooraf bepaalde verkorting behouden blijft. Na de operatie kan men namelijk direct belast worden met een speciaal ontworpen postoperatieve schoen.
Recenter heeft percutane chirurgie deze botdelen ( osteotomie ) veranderd door het ontbreken van fixaties, een systematische behandeling van de drie centrale vingers en een andere theoretische benadering. De losgemaakte koppen bewegen namelijk tijdens het lopen, totdat ze een evenwicht bereiken dat overeenkomt met een gelijkmatige belastingsverdeling. Het is dus de biomechanica van het lichaam zelf en niet de operatie die de optimale positie van de middenvoetsbeentjes bepaalt. Deze techniek heet DMMO (Distale Minimaal Invasieve Metatarsale Osteotomie).
NAZORG NA DE OPERATIE
Na een ingreep aan de middenvoetsbeentjes (klassieke Weil-osteotomie of percutane operatie) is meestal gedurende 6 weken een speciale orthopedische schoen nodig. De voet kan 1-3 maanden gezwollen en gevoelig blijven. Het ongemak neemt snel af zodra het bot volledig genezen is; röntgenfoto's zijn vereist tijdens de controleafspraken.
Minder intensieve sporten zoals zwemmen of fietsen kunnen 6 weken na de operatie worden hervat; hardlopen of contactsporten kunnen na 3 maanden worden hervat.
Autorijden is na 6 weken weer mogelijk. Wanneer er slechts één voet is geopereerd, mag er na kortere tijd weer worden gereden, mits het een automaat betreft.
Afhankelijk van het soort werk is doorgaans een periode van 2 tot 9 weken werkonbekwaamheid vereist.
RISICO'S EN COMPLICATIES
Naast de mogelijke complicaties na elke vorm van chirurgie (trombose, infectie <1%, algodystrofie <1%), kunnen de volgende complicaties optreden na een metatarsale osteotomie:
- Vertraagde of afwezigheid van botconsolidatie (zeer zeldzaam)
- Aanhoudende zwelling van de voet die langer dan 12 weken aanhoudt (vaak) en meestal spontaan verdwijnt
- Aanhoudende pijn (zeldzaam)
- De mogelijke risico's of complicaties bij andere procedures zijn afhankelijk van het type operatie en uw specialist zal u hierover uitgebreid informeren.
- Gewrichtsstijfheid . Dit komt vaak voor en moet worden beperkt door dagelijkse oefeningen in de vroege postoperatieve fase, te beginnen enkele weken na de operatie.
