dr Laurent Goubau
WAT IS HET?
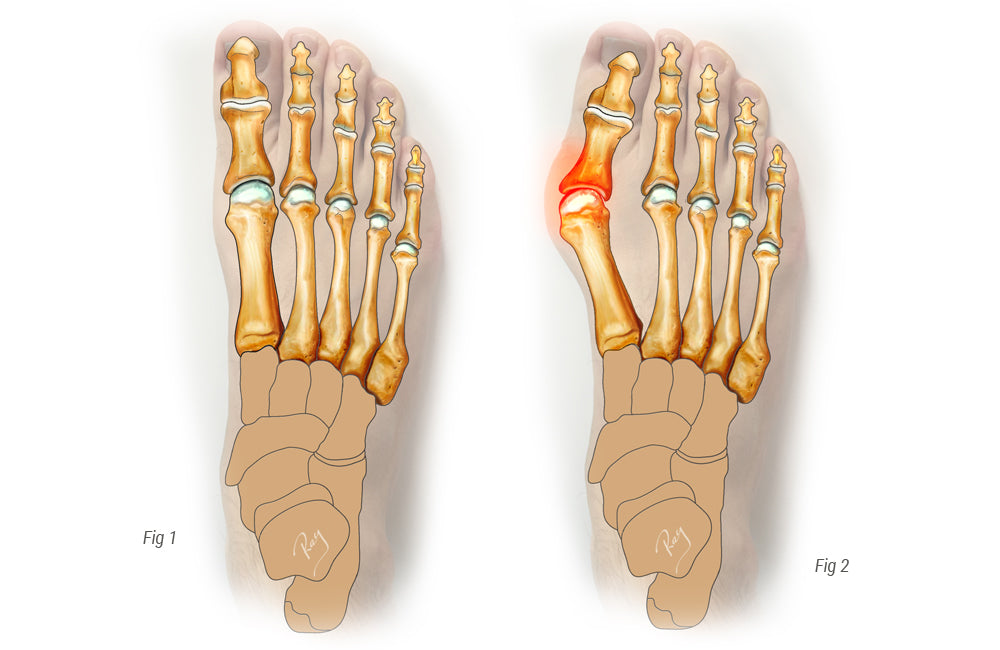
Hallux valgus, beter bekend als een "bunion", is een veel voorkomende progressieve misvorming van de voet. Het bestaat uit de rotatie van het eerste middenvoetsbeentje rond de basis en de verschuiving van de eerste teen naar de tweede. Dit resulteert in de ontwikkeling van een pijnlijke uitstulping aan de binnenkant van de voet (= bunion). Soms wordt gedacht dat dit een pijnlijke groei is die uit de rand van de voet groeit. Het is in feite een misvorming tussen het middenvoetsbeentje en het kootje die deze knobbel veroorzaakt. De knobbel ontstaat door de progressieve druk van het kopje van het middenvoetsbeentje tegen de huid.
Bij alle varianten van hallux valgus biedt het eerste middenvoetsbeentje onvoldoende ondersteuning. Een belangrijk deel van deze stabiliteit hangt samen met de juiste uitlijning van de pezen in de voeten en de hallux valgus verstoort, als gevolg van deze afwijking, de balans. Onder normale omstandigheden en in staande positie draagt het eerste middenvoetsbeentje twee keer zoveel gewicht als de andere middenvoetsbeentjes. Wanneer instabiliteit optreedt, wordt dit meestal opgemerkt tijdens het lopen of bij het belasten van de voet. In dergelijke gevallen ontvangt het betreffende middenvoetsbeentje slechts een fractie van het lichaamsgewicht. De rest van het gewicht wordt gedragen door de volgende middenvoetsbeentjes, die niet ontworpen zijn voor een dergelijke belasting. Om deze reden gaat hallux valgus vaak gepaard met pijn onder de voorvoet, waardoor de chronische belasting van de centrale middenvoetsbeentjes als gevolg van deze compensatieoverbelasting zichtbaar wordt (zie METATARSALGIE). Dit is nog duidelijker bij patiënten met aanzienlijke instabiliteit van de binnenste kolom (instabiele binnenste kolom, hypermobiele platvoet, enz.).
PRESENTATIE
Het grootste probleem bevindt zich meestal bij de benige uitsteeksels aan de binnenkant van de voet (= pseudo-exostosen). Dit veroorzaakt een conflict in de schoen, vooral bij het dragen van hoge hakken of smalle schoenen.
Zoals hierboven uitgelegd, gaat het bij veel gevallen van hallux valgus om een verschuiving van de belasting van het eerste middenvoetsbeentje naar de volgende middenvoetsbeentjes, wat pijn onder de voorvoet veroorzaakt (metatarsalgie). Dit is een veelvoorkomende klacht.
Wanneer de aandoening vergevorderd is en de misvorming verergert, komt de grote teen in contact met de tweede teen. Dit kan ook een bron van conflict worden.
WANNEER MOET U EEN SPECIALIST RAADPLEGEN?
Hoewel er niet-chirurgische behandelingsopties bestaan (zoals het vervangen van schoenen, enz.), is hallux valgus een progressieve aandoening en neemt het ongemak over het algemeen in de loop van de tijd toe. Artsen waren jarenlang van mening dat patiënten moesten wachten tot de pijn ondraaglijk werd voordat ze een consult zouden aanvragen; dit is echter momenteel niet meer het geval. Deze aanpak was inderdaad het geval toen de technieken niet erg effectief en bijzonder pijnlijk waren.
De situatie is inmiddels veranderd en als een hallux valgus te lang onbehandeld blijft, kunnen er andere aandoeningen ontstaan (zoals artritis, hamertenen, etc.) of kan er een complexere corrigerende operatie nodig zijn.
Wij adviseren om een specialist te raadplegen wanneer de klachten een verandering in de kwaliteit van leven of normale activiteiten teweegbrengen, wanneer het aantrekken van schoenen moeilijk wordt of wanneer de misvorming snel verergert.
NIET-CHIRURGISCHE BEHANDELING
Omdat de pijn voornamelijk wordt veroorzaakt door de knobbel die tegen de schoen drukt, is het veranderen van het type schoeisel uiteraard de eerste stap. Zachte en brede schoenen hebben de voorkeur, evenals schoenen zonder plaatselijke en overmatige drukpunten. Het dragen van hoge hakken moet worden beperkt, omdat deze de belasting op de voorvoet vergroten en een conflict in de schoen veroorzaken.
Het dragen van op maat gemaakte inlegzolen kan in de beginfase van de aandoening helpen.
Er zijn nachtspalken op de markt die helpen de grote teen recht te zetten. De werkzaamheid ervan is echter nog niet vastgesteld en hun nut lijkt beperkt te zijn tot pijnverlichting en corrigeert niet de hallux valgus-deformiteit.
CHIRURGISCHE BEHANDELING
Wanneer conservatieve behandeling niet voldoende is, moet een operatie worden voorgesteld.
Er zijn meer dan 180 verschillende procedures beschikbaar om een hallux valgus te corrigeren. Hoewel sommige van deze procedures niet meer passen in de moderne aanpak van deze aandoening, omvatten de meeste een operatie aan het eerste middenvoetsbeentje. Het hoofddoel is om het gewricht tussen het middenvoetsbeentje en het kootje terug te brengen naar de oorspronkelijke positie, waardoor de teen opnieuw wordt uitgelijnd en de omliggende pezen opnieuw worden gecentreerd. Het bot wordt meestal doorgesneden (osteotomie) om de kop van het middenvoetsbeentje naar de gewenste positie te verplaatsen. De meeste technieken variëren wat betreft de specifieke werking op het bot, de richting van de osteotomie en de vorm of lengte ervan.
Een operatie kan aan beide kanten tegelijk worden uitgevoerd. In dat geval kan het herstel iets langzamer verlopen.
Een techniek die Scarf -procedure wordt genoemd, is een van de meest populaire. Deze bestaat uit het maken van een Z-vormige incisie (Scarf) in het middenvoetsbeentje om de grote teen opnieuw uit te lijnen. Om de positie te behouden, wordt de incisie (osteotomie) vastgezet met schroeven of met een speciale osteotomietechniek zonder fixatie. Deze ingreep wordt meestal uitgevoerd via een open operatie.
Het is mogelijk om deze operatie uit te voeren met een percutane minimaal invasieve chirurgische techniek. Dit is een nieuwe aanpak, waarbij een kleine, enkele incisie van 1 mm wordt gemaakt. De osteotomie zelf is identiek aan een open operatie, maar de minimale incisie zorgt voor een sneller herstel, vrijwel onzichtbare littekens en beperkte pijn. De fixatie wordt uitgevoerd met schroeven of een metalen pin met een diameter van 2 mm, die 4-5 weken na de operatie wordt verwijderd. Deze verwijdering is pijnloos en wordt uitgevoerd in de praktijk van de arts.
Tot slot is in gevallen met een significante instabiliteit van het eerste middenvoetsbeentje, tijdens bepaalde chirurgische revisies of bij een ernstige misvorming, een metatarsale osteotomie niet voldoende en is het risico op recidief hoog. In deze gevallen is een operatie aan de basis van het middenvoetsbeentje de voorkeursoptie. Het kraakbeen van het gewricht tussen het wiggenbeen en het middenvoetsbeentje wordt verwijderd en de twee botten worden met een plaat in nauw contact gebracht, waardoor de fusie van dit gewricht in een uitgelijnde positie mogelijk wordt. Dit is een artrodese, dat wil zeggen een fusie van het gewricht (Lapidus artrodese).
Hoe dan ook, uw chirurg zal met u de beste chirurgische optie bespreken. Elke voet is anders en vereist specifieke zorg voor een optimale en duurzame correctie.
NAZORG NA DE OPERATIE
Lopen met gewicht is per direct toegestaan, mits beschermd met speciale schoenen gedurende zes weken. Een wandelstok mag uitsluitend voor comfortdoeleinden worden gebruikt.
Bij een percutane operatie met een pin wordt deze na 4-5 weken verwijderd. Regelmatige controles (1 week, 3 weken, 6 weken en 3 maanden) gedurende deze periode zorgen mogelijk voor een complicatievrije genezing.
Autorijden kan na zes weken weer hervat worden. Wanneer er slechts één voet geopereerd is, mag er na kortere tijd weer autorijden, mits het een automaat betreft.
Afhankelijk van het beroep (zittend of actief werk, staand werk of niet, etc.) is het 3 weken tot 3 maanden duren voordat u weer aan het werk kunt.
Wat betreft de sport kunt u na 6 weken beginnen met zwemmen of fietsen; hardlopen of contactsporten vereisen minimaal 3 maanden.
Het dragen van schoenen met hoge hakken is over het algemeen toegestaan vanaf de vierde maand.
RISICO'S EN COMPLICATIES
Naast de mogelijke complicaties na elke vorm van chirurgie (trombose, infectie <1%, algodystrofie <1%), wordt erkend dat de behandeling van hallux valgus de volgende risico's en complicaties met zich meebrengt:
- Terugkeer van de misvorming (4-10%). Dit kan te wijten zijn aan een foutieve analyse van het probleem, een technisch defect, een onjuiste indicatie of het niet opvolgen van de postoperatieve instructies.
- Niet-verbinding van de botsnede of artrodese (pseudoartrose), zeldzame aandoening
- Zenuwbeschadiging (meestal tijdelijk en regressief)
- Aanhoudende zwelling (oedeem). Normaal gedurende de eerste 2-3 maanden, maar kan in sommige gevallen langer aanhouden.
- Stijfheid (vaak). Elke ingreep aan een gewricht veroorzaakt stijfheid, waardoor mobilisatie na de operatie door een fysiotherapeut of de patiënt noodzakelijk is.
