dr Laurent Goubau
WAT IS HET?
Hamerteen is een veelvoorkomende aandoening aan de tenen die vooral vrouwen boven de 50 treft. Afhankelijk van de vorm van de tenen wordt het een klauw- of hamerteen genoemd, afhankelijk van de aangetaste gewrichten. Met de toenemende kennis over dit onderwerp verliest deze classificatie geleidelijk aan relevantie en ligt de focus nu op het bepalen van de flexibele, semi-rigide of rigide aard van de teen, afhankelijk van het vermogen van de teen om gemakkelijk zijn normale positie terug te krijgen.
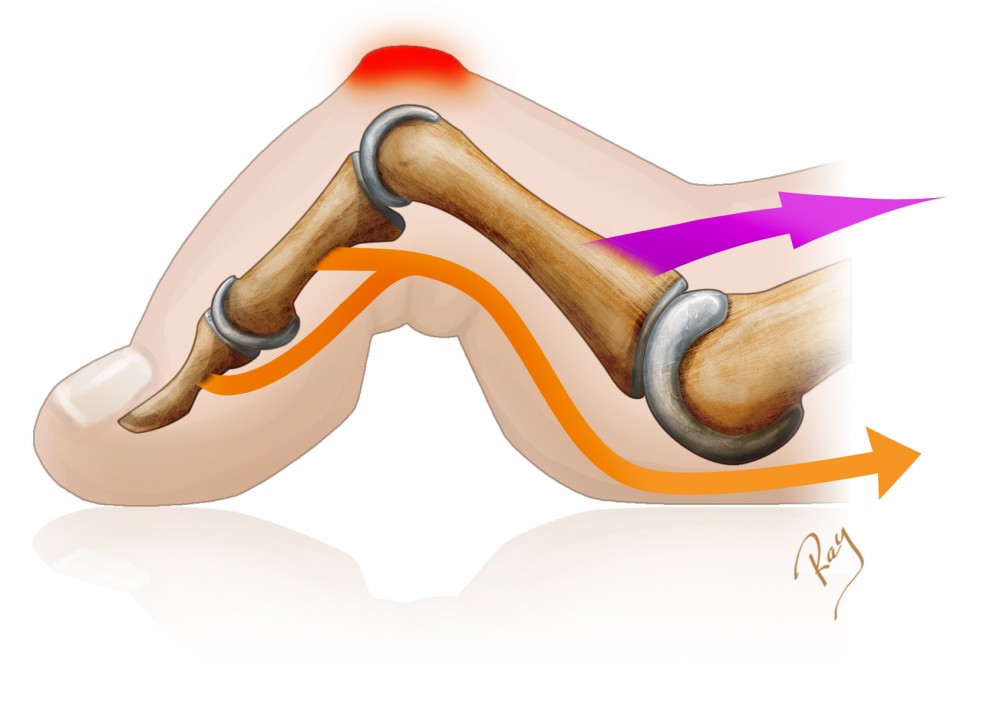
De teen bevindt zich normaal gesproken in een gestrekte positie en dit is in wezen afhankelijk van het evenwicht tussen de pezen in de voet. Pezen die aan de vingerkootjes vastzitten, zorgen voor de mobiliteit van de verschillende gewrichten en maken de flexie of extensie van elk gewricht mogelijk. Het is een delicaat evenwicht waarbij elke pees compensatie van de andere pezen moet ontvangen, zodat de teen in zijn normale rustpositie blijft.
Als een van deze pezen sterker is of in de loop der tijd gewoonweg korter is geworden, treedt er al snel een misvorming op in flexie of extensie als gevolg van de disbalans tussen de pezen en het onvermogen van het lichaam om de retractie te compenseren. De vorm van de teen hangt dan af van de aangedane pees(en).
Meestal is het eerste teken een terugtrekking van de buigspieren van de teen, wat een flexie van het eerste interfalangeale gewricht veroorzaakt. Hierna kan zich een misvorming van het metatarsofalangeale gewricht aan de basis van de teen ontwikkelen, wat de teen zijn karakteristieke hamervorm geeft. In deze positie zal de teen snel oncomfortabel aanvoelen bij het dragen van schoenen vanwege de overmatige druk tussen het interfalangeale gewricht en de schoen. Er zal dan een likdoorn (of callus) ontstaan, een verdikking van de huid die de teen tegen deze druk beschermt.
Hoewel de misvorming van het gewricht aanvankelijk kan afnemen, zal deze geleidelijk leiden tot verstijving en steeds moeilijker te verdragen worden. Uiteindelijk kan een ontwrichting van de teenbasis worden waargenomen. Dit type geval is de ernstigste vorm en veroorzaakt meestal pijn onder de voet.
Hoewel deze misvormingen zich in een geïsoleerde vorm kunnen voordoen, zijn ze over het algemeen gekoppeld aan andere aandoeningen. De meest voorkomende aandoening is hallux valgus (knobbel), die systematisch leidt tot overbelasting van aangrenzende tenen en de retractie van de teenpezen en daarmee hun misvorming aanzienlijk vergemakkelijkt. Andere oorzaken van hamertenen zijn onder andere een hoge voetboog, neuropathie van de voet, reumatoïde artritis,... Het dragen van hoge hakken, verkeerd schoeisel of een Griekse voet (waarbij de tweede teen langer is dan de eerste) zijn andere omstandigheden die kunnen leiden tot het ontstaan van hamertenen, hetzij door een verkeerde positie van de tenen in schoenen, hetzij door overbelasting van de voorvoet.
KLINISCHE PRESENTATIE
De dorsale druk van de schoen op de teen is meestal de eerste klacht. Bij rigide misvormingen kan de likdoorn beschadigd raken, een zweer vormen en uiteindelijk geïnfecteerd raken. Dit is een belangrijk waarschuwingssignaal, vooral bij diabetespatiënten bij wie de tenen een belangrijke bron van complicaties zijn.
Ernstige gevallen van hamertenen leiden tot drukveranderingen op het eindpunt van de teen. Normaal gesproken wordt de last op het puntje van de teen gedragen door het vlezige deel (de teen-grond-ondersteuning). Bij hamertenen drukt de teen op het meest eindpunt (de apicale ondersteuning), wat hiervoor totaal ongeschikt is en hevige pijn veroorzaakt.
Ten slotte, wanneer het metatarsofalangeale gewricht is aangedaan, treedt vaak gewrichtspijn (tweedevingersyndroom) op als gevolg van de instabiliteit van het gewricht. Als deze instabiliteit voortschrijdt, kan een gedeeltelijke ontwrichting, gevolgd door een volledige ontwrichting van de falanx optreden als gevolg van het falen van de plantaire plaat. In dergelijke gevallen wordt er aanzienlijke druk overgebracht op het middenvoetsbeentje, waardoor de belasting op dit niveau toeneemt, wat een klassieke vorm van metatarsalgie veroorzaakt.
WANNEER MOET U EEN SPECIALIST RAADPLEGEN?
Wanneer de hamerteen een pijnlijke druk in de schoen veroorzaakt of wanneer het middenvoetsbeentje gevoelig wordt, is het zeer raadzaam om een specialist te raadplegen.
De tenen van diabetespatiënten moeten regelmatig worden gecontroleerd. Patiënten moeten altijd contact opnemen als er huidletsels of verwondingen optreden.
NIET-CHIRURGISCHE BEHANDELING
Conservatieve behandeling bestaat voornamelijk uit het aanpassen van het schoeisel. Zachte en comfortabele schoenen, zonder drukpunten, hebben de voorkeur. Het dragen van smalle schoenen of schoenen met hoge hakken verergert de symptomen en dient te worden vermeden.
Behandeling door een podotherapeut omvat de meeste niet-chirurgische opties. Het verwijderen van eeltplekken kan de symptomen vaak aanzienlijk verminderen. Siliconen steunzolen kunnen worden gebruikt, omdat ze de misvorming gedeeltelijk verminderen (alleen bij flexibele tenen) en bescherming bieden tegen druk en wrijving.
CHIRURGISCHE BEHANDELING
Wanneer conservatieve behandeling niet langer voldoende is, moet een operatie worden voorgesteld.
Conventionele correctietechnieken bestaan uit het uitvoeren van een artrodese van het proximale interfalangeale gewricht, dat wil zeggen het verwijderen van het kraakbeen en het plaatsen van pinnen terwijl het gebied geneest.
Minimaal invasieve technieken zijn recentelijk op de markt gekomen. Deze technieken zijn uitstekend geschikt voor correcties met minimale incisies, zonder dat er pinnen nodig zijn en waarbij het gewricht over het algemeen behouden blijft. Wij geven de voorkeur aan dergelijke technieken. De benodigde procedure is afhankelijk van het type afwijking en verschilt per geval. Indien nodig worden de verkorte pezen verlengd of selectief doorgesneden om de juiste balans van de pezen te herstellen. Deze ingrepen kunnen worden aangevuld met een sectie (osteotomie) in een of meerdere vingerkootjes om de teen te verkorten en de teen opnieuw te richten. Tot slot kunnen, afhankelijk van het type afwijking, ook andere technieken tegelijkertijd worden uitgevoerd (capsulotomie, botverwijdering, ...). Het is belangrijk om de indicaties en beperkingen van deze technieken te kennen; de chirurg zal u elke techniek in detail uitleggen.
NAZORG NA DE OPERATIE
Bij percutane correctie is het verband bijzonder belangrijk, omdat het de tenen perfect van richting verandert en ervoor zorgt dat ze in de juiste positie genezen. De chirurg of verpleegkundige verwisselt het verband één week en drie weken na de operatie. De teen heeft gedurende zes weken begeleiding nodig.
Patiënten krijgen orthopedische schoenen ; lopen is echter ook mogelijk op brede, comfortabele schoenen (sportschoenen, enz.).
Direct na de operatie en zodra u weer volledige controle over uw onderste ledematen heeft (bij locoregionale anesthesie), kunt u weer lopen en uw volledige gewicht dragen.
Meestal is een behandeling met fysiotherapie niet nodig, maar patiënten wordt wel gevraagd om dagelijks hun tenen te mobiliseren om stijfheid te voorkomen.
Autorijden is na enkele weken, na het verwijderen van de medische schoen, weer toegestaan. Wanneer slechts één voet is geopereerd, mag men direct autorijden, mits het een automaat betreft.
Afhankelijk van de operatietechniek en het beroep van de patiënt is een ziekteverlof van 1 tot 4 weken vereist.
Contactloze sporten kunnen na zes weken worden hervat. Over het algemeen kunnen alle activiteiten vanaf de derde maand worden hervat.
RISICO'S EN COMPLICATIES
Naast de mogelijke complicaties na elke vorm van chirurgie (trombose, infectie <1%, algodystrofie <1%), wordt erkend dat de behandeling van hamertenen de volgende risico's en complicaties met zich meebrengt:
- Terugkeer van de misvorming . Dit hangt af van de ernst van het letsel, de operatietechniek en de oorzaak van de misvorming. Mogelijk is een nieuwe operatie nodig.
- Zenuwbeschadiging . Relatief vaak voorkomend, maar meestal spontaan regressief.
- Verlies van mobiliteit in de teen . Omdat de misvorming te wijten is aan verkorting van de pezen, leidt verlenging of spleetvorming vaak tot verminderde mobiliteit. Dit gevoel kan tijdelijk zijn en wordt over het algemeen goed verdragen.
- Gewrichtsstijfheid . Dit komt vaak voor en moet beperkt worden door dagelijkse oefeningen, te beginnen enkele weken na de operatie.
